BPD Có Thể Được Chữa Khỏi Không? Làm Bài Kiểm Tra BPD Miễn Phí để Khám phá Con đường Phục hồi và Tỷ lệ Thành công
December 15, 2025 | By Isabella Rossi
Đối với nhiều người đang trải qua những cảm xúc mãnh liệt của Rối loạn nhân cách ranh giới (BPD), hoặc đối với những người nghi ngờ mình mắc phải, một câu hỏi nặng trĩu thường lởn vởn trong đầu: Đây có phải là một bản án chung thân không? Nỗi sợ rằng những cơn bão cảm xúc, các mối quan hệ không ổn định và cảm giác trống rỗng sẽ không bao giờ kết thúc có thể rất choáng ngợp. Bài viết này nhằm mục đích cung cấp một câu trả lời rõ ràng và đầy hy vọng.
Quan niệm về BPD đang thay đổi. Điều từng được xem là một tình trạng không thể chữa khỏi giờ đây được hiểu là một rối loạn có những lộ trình phục hồi rõ ràng. Chúng ta sẽ khám phá ý nghĩa thực sự của "hồi phục", xem xét các phương pháp điều trị dựa trên bằng chứng tạo nên sự thay đổi bền vững và thảo luận về khả năng thực sự xây dựng một cuộc sống ổn định, viên mãn. Nếu bạn chỉ mới bắt đầu khám phá những cảm xúc này, bước đầu tiên tuyệt vời là hiểu các triệu chứng của bạn. Bạn có thể bắt đầu hành trình đó với bài kiểm tra BPD bảo mật của chúng tôi.
Hiểu về Hồi phục BPD: "Chữa khỏi" Có nghĩa là gì?
Khi chúng ta nói về bệnh thể chất, từ "chữa khỏi" thường có nghĩa là bệnh đã hoàn toàn biến mất. Với các tình trạng sức khỏe tâm thần như BPD, khái niệm này có sắc thái hơn. Thay vì "chữa khỏi", các chuyên gia thường sử dụng thuật ngữ "thuyên giảm". Điều này không có nghĩa là làm ngơ trước những thách thức đã qua; nó có nghĩa là đạt đến một điểm mà bạn không còn đáp ứng các tiêu chí chẩn đoán cho rối loạn và có thể hoạt động hiệu quả trong cuộc sống hàng ngày.
Hồi phục có nghĩa là quản lý cảm xúc của bạn tốt hơn. Nó xây dựng các mối quan hệ ổn định. Và nó giúp bạn phát triển một cảm nhận vững chắc về bản thân. Đó là một hành trình tiếp thu các kỹ năng mới và chữa lành những vết thương trong quá khứ, dẫn đến một cuộc sống cân bằng và ý nghĩa.
Có thể Đạt được Sự Thuyên giảm Hoàn toàn cho Rối loạn nhân cách ranh giới không?
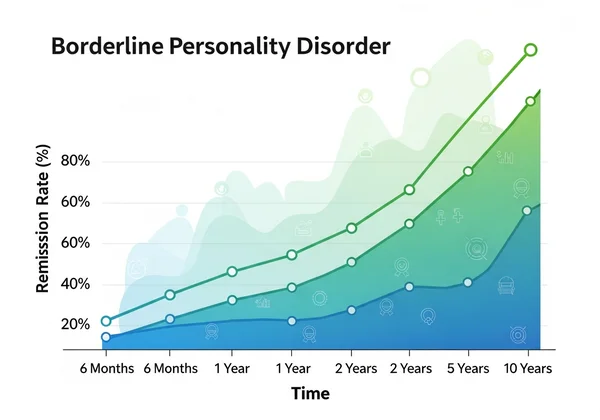
Vâng, hoàn toàn có thể. Đây là thông điệp đầy hy vọng nhất từ nghiên cứu hiện đại. Các nghiên cứu dài hạn đã cho thấy tỷ lệ hồi phục BPD cao đáng ngạc nhiên. Ví dụ, nghiên cứu từ các tổ chức như Bệnh viện McLean đã phát hiện ra rằng sau khoảng 10 năm, đa số đáng kể các cá nhân được chẩn đoán mắc BPD không còn đáp ứng các tiêu chí của rối loạn.
Sự thuyên giảm hoàn toàn làm dịu đi các triệu chứng cốt lõi. Hãy nghĩ đến nỗi sợ bị bỏ rơi điên cuồng, thay đổi tâm trạng dữ dội và cảm giác trống rỗng kinh niên. Chúng trở nên có thể quản lý được. Điều đó có nghĩa là bạn có thể vượt qua những thách thức của cuộc sống mà không bị cuốn đi bởi sự rối loạn điều hòa cảm xúc. Đây không phải là một kết quả hiếm gặp; với phương pháp điều trị và hỗ trợ đúng đắn, đó là một mục tiêu thực tế và có thể đạt được đối với nhiều người.
Các Yếu tố Chính Tác động đến Kết quả và Tỷ lệ Thành công khi Phục hồi BPD
Mỗi hành trình hồi phục là độc nhất, nhưng một số yếu tố chính được biết là ảnh hưởng đến kết quả tích cực và cải thiện sự thành công trong thuyên giảm BPD. Hiểu những điều này có thể tiếp thêm sức mạnh cho bạn trên con đường của mình.
- Chẩn đoán Sớm và Chính xác: Bạn càng hiểu rõ mình đang đối phó với điều gì sớm bao nhiêu, bạn càng có thể bắt đầu điều trị hiệu quả sớm bấy nhiêu.
- Cam kết Trị liệu: Hồi phục đòiRoutine hỏi sự tham gia tích cực. Tham dự các buổi trị liệu và thực hành các kỹ năng giữa các buổi hẹn là rất quan trọng.
- Loại Trị liệu Phù hợp: Không phải tất cả các liệu pháp đều hiệu quả như nhau đối với BPD. Tìm một nhà trị liệu được đào tạo về các phương pháp điều trị dựa trên bằng chứng như DBT là rất quan trọng.
- Hệ thống Hỗ trợ Vững mạnh: Có gia đình, bạn bè hoặc đối tác thấu hiểu có thể tạo ra sự khác biệt lớn.
- Giải quyết các Tình trạng Đồng thời: BPD thường đi kèm với các tình trạng khác như trầm cảm, lo âu hoặc rối loạn sử dụng chất gây nghiện. Điều trị đồng thời những tình trạng này là cần thiết cho hạnh phúc tổng thể.
Các Con đường Điều trị Dựa trên Bằng chứng để Thay đổi Bền vững
Khoa học mang lại cho chúng ta lý do thực sự để hy vọng—hàng thập kỷ nghiên cứu đã củng cố những phương pháp này. Các nhà nghiên cứu đã xác định các phương pháp trị liệu hiệu quả cao nhắm cụ thể vào những khó khăn cốt lõi của BPD. Những phương pháp điều trị này cung cấp các công cụ và chiến lược cần thiết để quản lý triệu chứng và xây dựng một cuộc sống đáng sống.
Nền tảng: Liệu pháp Hành vi Biện chứng (DBT) và Hiệu quả của nó
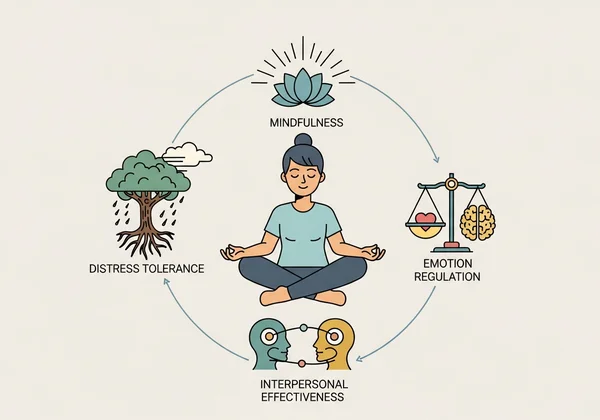
Nếu có một phương pháp điều trị tiêu chuẩn vàng cho BPD, đó chính là Liệu pháp Hành vi Biện chứng (DBT). Được phát triển bởi Tiến sĩ Marsha Linehan, DBT được thiết kế đặc biệt để điều trị sự rối loạn điều hòa cảm xúc mãn tính và các hành vi tự hủy hoại bản thân liên quan đến BPD.
DBT dạy bốn kỹ năng chính.
- Đầu tiên, chánh niệm: Giữ sự hiện diện mà không phán xét.
- Thứ hai, khả năng chịu đựng khó khăn: Đối phó với nỗi đau và khủng hoảng mà không làm cho tình hình tệ hơn.
- Thứ ba, điều hòa cảm xúc: Hiểu và quản lý những cảm xúc mãnh liệt một cách lành mạnh hơn.
- Thứ tư, hiệu quả tương tác cá nhân: Học cách truyền đạt nhu cầu của bạn, thiết lập ranh giới và xây dựng các mối quan hệ tích cực.
Hiệu quả của DBT được hỗ trợ bởi nhiều nghiên cứu, cho thấy nó giảm đáng kể hành vi tự làm hại bản thân, nhập viện và tỷ lệ bỏ trị liệu trong khi cải thiện chất lượng cuộc sống tổng thể.
Các Liệu pháp Hiệu quả Khác: Liệu pháp Sơ đồ, MBT và các Thích ứng CBT
Mặc dù DBT là phương pháp nổi tiếng nhất, nhưng nó không phải là lựa chọn duy nhất. Các liệu pháp khác cũng đã được chứng minh là hiệu quả trong việc giúp các cá nhân đạt được sự thuyên giảm BPD.
- Liệu pháp Sơ đồ: Liệu pháp này tập trung vào việc xác định và thay đổi các khuôn mẫu tư duy, cảm xúc và hành vi tiêu cực lâu dài (gọi là "sơ đồ") thường bắt đầu từ thời thơ ấu.
- Liệu pháp Dựa trên Tâm thần hóa (MBT): MBT giúp các cá nhân hiểu rõ hơn về trạng thái tinh thần của bản thân và người khác—suy nghĩ, cảm xúc và ý định. Điều này cải thiện nhận thức về bản thân và sự ổn định trong mối quan hệ.
- Các Thích ứng của Liệu pháp Hành vi Nhận thức (CBT): Mặc dù CBT tiêu chuẩn có thể kém hiệu quả hơn đối với BPD, nhưng các thích ứng chuyên biệt có thể giúp giải quyết các khuôn mẫu tư duy sai lệch góp phần gây ra đau khổ về cảm xúc.
Vai trò của Thuốc trong Quản lý Triệu chứng BPD
Một câu hỏi phổ biến là liệu thuốc có thể "chữa khỏi" BPD không. Hiện tại, không có loại thuốc đơn lẻ nào được phê duyệt đặc biệt để điều trị toàn bộ BPD. Tuy nhiên, thuốc có thể đóng một vai trò hỗ trợ quan trọng trong quản lý BPD dài hạn.
Một bác sĩ tâm thần có thể kê thuốc để nhắm vào các triệu chứng cụ thể hoặc các tình trạng đồng thời. Điều này có thể bao gồm:
- Thuốc ổn định tâm trạng để giúp giảm tính bốc đồng và thay đổi tâm trạng.
- Thuốc chống trầm cảm để điều trị trầm cảm đồng thời.
- Thuốc chống loạn thần (thường ở liều thấp) để giúp với suy nghĩ không có tổ chức hoặc tức giận.
Thuốc có hiệu quả tốt nhất khi kết hợp với trị liệu. Trị liệu xây dựng các kỹ năng sống bạn cần để thay đổi bền vững.
Quản lý Dài hạn & Xây dựng Cuộc sống Đáng sống
Hồi phục từ BPD không phải là một sự kiện một lần mà là một quá trình phát triển và tự chăm sóc bản thân liên tục. Sau liệu pháp chuyên sâu, trọng tâm chuyển sang quản lý BPD dài hạn và tích hợp những thói quen lành mạnh vào cuộc sống hàng ngày của bạn. Đây là lúc bạn thực sự bắt đầu xây dựng một cuộc sống chân thực và đúng nghĩa viên mãn.
Nếu bạn chỉ mới bắt đầu tự hỏi về các khuôn mẫu cảm xúc của mình, bài kiểm tra trực tuyến miễn phí của chúng tôi có thể là một điểm khởi đầu hữu ích, riêng tư để tự suy ngẫm.
Trau dồi Kỹ năng Đối phó Bền vững và Điều hòa Cảm xúc
Các kỹ năng học được trong trị liệu, đặc biệt là DBT, không chỉ dành cho những lúc khủng hoảng. Chúng trở thành bộ công cụ hàng ngày của bạn để điều hướng cuộc sống. Điều này có nghĩa là thực hành chánh niệm khi bạn cảm thấy căng thẳng, sử dụng các kỹ năng chịu đựng khó khăn để vượt qua thời điểm khó khăn, và áp dụng các kỹ thuật điều hòa cảm xúc để ngăn chặn những phiền toái nhỏ biến thành những cơn bão cảm xúc. Theo thời gian, những kỹ năng này trở thành bản năng thứ hai, tạo ra một nền tảng mới, ổn định hơn cho đời sống cảm xúc của bạn.
Xây dựng Mối quan hệ Lành mạnh và Hệ thống Hỗ trợ Vững mạnh
Các mối quan hệ thường là trung tâm của cuộc đấu tranh đối với những người mắc BPD. Một phần quan trọng của quá trình hồi phục dài hạn là học cách xây dựng và duy trì các mối quan hệ lành mạnh. Điều này bao gồm:
- Giao tiếp Hiệu quả: Diễn đạt rõ ràng nhu cầu và cảm xúc của bạn mà không đổ lỗi hay buộc tội.
- Thiết lập Ranh giới: Hiểu giới hạn của bạn và tôn trọng truyền đạt chúng cho người khác.
- Chọn những Người Hỗ trợ: Bao quanh bản thân với những cá nhân thấu cảm, đáng tin cậy và tôn trọng hành trình hồi phục của bạn.
Hành trình đến Chấp nhận Bản thân và Giảm Kỳ thị
Cuối cùng, sự hồi phục lâu dài liên quan đến việc thay đổi mối quan hệ của bạn với chính mình. Điều này có nghĩa là buông bỏ sự xấu hổ và tự phê bình thường đi kèm với chẩn đoán BPD. Đó là về việc học cách đối xử với bản thân bằng sự trắc ẩn và thấu hiểu tương tự như bạn sẽ dành cho một người bạn. Chấp nhận bản thân không phải là trở nên hoàn hảo; đó là về việc thừa nhận những đấu tranh trong quá khứ đồng thời đón nhận giá trị vốn có và khả năng phát triển của bạn.
Con đường đến Hy vọng của Bạn: Hồi phục từ Rối loạn nhân cách ranh giới
Vậy, BPD có thể được chữa khỏi không? Câu trả lời là một khẳng định mạnh mẽ—hồi phục xảy ra đối với rất nhiều người. Mặc dù từ "chữa khỏi" có thể không phải là từ hoàn hảo nhất, nhưng đạt được sự thuyên giảm hoàn toàn và xây dựng một cuộc sống ổn định, ý nghĩa là một thực tế đối với vô số người.
Hồi phục là một hành trình học các kỹ năng mới, chữa lành những vết thương cũ và khám phá sức mạnh của bản thân. Nó đòi hỏi sự cam kết, nhưng với các phương pháp điều trị hiệu quả, dựa trên bằng chứng như DBT và một hệ thống hỗ trợ vững mạnh, bạn có thể vượt lên trên việc chỉ tồn tại và bước vào một cuộc sống nơi bạn phát triển thịnh vượng.
Nếu bạn đang đọc bài viết này vì bạn thấy mình hoặc người thân có các triệu chứng của BPD, hãy biết rằng đây là bước đầu tiên của bạn trên con đường hướng tới hy vọng. Để có được sự rõ ràng hơn, bạn có thể bắt đầu bài kiểm tra của mình ngay bây giờ. Nó miễn phí, bảo mật và được thiết kế để giúp bạn hiểu các khuôn mẫu cảm xúc của mình.
Tuyên bố miễn trừ trách nhiệm: Bài viết này chỉ dành cho mục đích thông tin và không cấu thành lời khuyên y tế. Nội dung không nhằm mục đích thay thế cho chẩn đoán hoặc điều trị chuyên nghiệp. Bài kiểm tra BPD miễn phí của chúng tôi là một công cụ sàng lọc, không phải công cụ chẩn đoán. Luôn tìm kiếm lời khuyên từ chuyên gia sức khỏe tâm thần đủ trình độ nếu bạn có bất kỳ câu hỏi nào liên quan đến tình trạng sức khỏe. Nếu bạn đang trong khủng hoảng, vui lòng liên hệ với đường dây nóng khủng hoảng hoặc đến phòng cấp cứu gần nhất.
Điểm Chính
BPD có thực sự được chữa khỏi không, hay nó luôn là một cuộc đấu tranh suốt đời?
BPD không phải là một bản án chung thân. Nghiên cứu cho thấy một tỷ lệ cao các cá nhân đạt được "thuyên giảm", nghĩa là họ không còn đáp ứng các tiêu chí chẩn đoán. Thông qua liệu pháp hiệu quả như DBT, mọi người học các kỹ năng để quản lý cảm xúc và xây dựng cuộc sống ổn định, giảm đáng kể cuộc đấu tranh hàng ngày.
Tỷ lệ thành công điển hình cho điều trị và thuyên giảm BPD là gì?
Tỷ lệ thành công rất đáng khích lệ. Các nghiên cứu dài hạn chỉ ra rằng có tới 85% cá nhân mắc BPD có thể đạt được sự thuyên giảm trong vòng 10 năm kể từ khi được chẩn đoán. Với phương pháp điều trị nhất quán, dựa trên bằng chứng, nhiều người thấy sự cải thiện đáng significant về các triệu chứng và chất lượng cuộc sống sớm hơn nhiều.
Làm thế nào tôi có thể được xét nghiệm chính thức cho Rối loạn nhân cách ranh giới?
Để có chẩn đoán chính thức, cần có một đánh giá toàn diện từ một chuyên gia sức khỏe tâm thần đủ trình độ, chẳng hạn như bác sĩ tâm thần hoặc nhà tâm lý học lâm sàng. Quá trình này thường bao gồm một cuộc phỏng vấn chi tiết về các triệu chứng, tiền sử cá nhân và kinh nghiệm của bạn. Mặc dù một công cụ sàng lọc trực tuyến có thể là bước đầu tiên hữu ích để xác định các triệu chứng tiềm ẩn, bạn có thể làm bài kiểm tra của chúng tôi để thu thập thông tin chi tiết trước khi nói chuyện với chuyên gia.
9 triệu chứng được sử dụng để chẩn đoán BPD là gì?
Chẩn đoán BPD được thực hiện bởi một nhà lâm sàng khi một người thể hiện ít nhất năm trong số chín triệu chứng sau đây, như được nêu trong DSM-5:
- Nỗ lực điên cuồng để tránh bị bỏ rơi có thật hoặc tưởng tượng.
- Một hình mẫu các mối quan hệ giữa các cá nhân không ổn định và mãnh liệt.
- Rối loạn nhận dạng: hình ảnh bản thân hoặc cảm nhận về bản thân không ổn định rõ rệt và dai dẳng.
- Bốc đồng ở ít nhất hai lĩnh vực có khả năng tự gây hại (ví dụ: chi tiêu, tình dục, lạm dụng chất gây nghiện, lái xe liều lĩnh, ăn uống vô độ).
- Hành vi tự tử tái diễn, cử chỉ, đe dọa, hoặc hành vi tự gây thương tích.
- Không ổn định cảm xúc do phản ứng rõ rệt của tâm trạng (ví dụ: rối loạn khí sắc dữ dội từng đợt, cáu kỉnh hoặc lo lắng thường kéo dài vài giờ).
- Cảm giác trống rỗng mãn tính.
- Cơn giận không thích hợp, dữ dội hoặc khó kiểm soát cơn giận.
- Ý tưởng hoang tưởng thoáng qua, liên quan đến căng thẳng hoặc các triệu chứng phân ly nặng.