BPD Test & Comorbidity: Understanding Overlap with Anxiety, Depression & PTSD
November 20, 2025 | By Isabella Rossi
Introduction: Navigating the Complexities: When BPD isn't Alone
Do your intense emotions feel like more than just anxiety or depression? You're not alone. This complex inner world is a common experience. Borderline Personality Disorder (BPD) frequently co-occurs with other mental health conditions, a phenomenon known as BPD comorbidity. This overlap can make understanding your symptoms and seeking the right treatment feel incredibly challenging. Do I have BPD test is a question that often arises when symptoms don't neatly fit into one box.
The primary struggle is often distinguishing BPD symptoms from, or understanding their interaction with, conditions like major depressive disorder, anxiety disorders, or post-traumatic stress disorder (PTSD). This guide illuminates these common overlaps, helping you recognize the signs, understand the connections, and see why a comprehensive assessment is vital for clarity and healing. Taking a preliminary step, like an online BPD assessment, can be a valuable starting point on your journey to understanding.
Understanding BPD Comorbidity: More Than One Diagnosis
The path to understanding your mental health is rarely a straight line. Grasping the concept of comorbidity is crucial to see the full picture, empowering you to seek the most effective, integrated care.
What Does "Comorbidity" Mean for Borderline Personality Disorder?
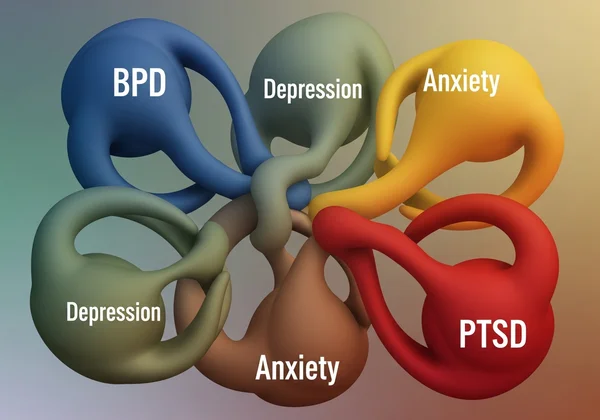
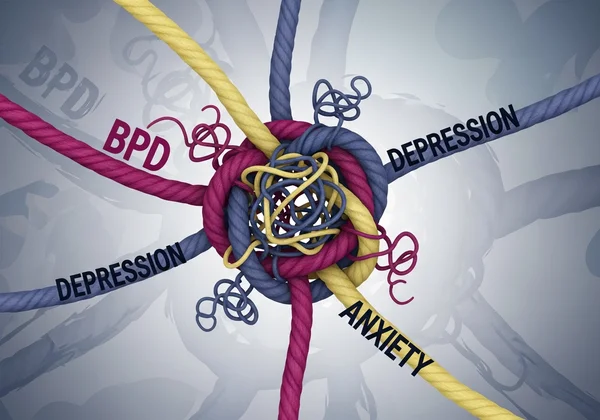
Comorbidity in mental health means a person has more than one diagnosis simultaneously. For individuals with Borderline Personality Disorder, this is the rule rather than the exception. Research consistently shows that BPD has high rates of comorbidity with other conditions, particularly mood disorders, anxiety disorders, and trauma-related disorders. These conditions often interact, influencing and intensifying one another. Understanding this interplay is the first step toward untangling your experiences.
Why Do BPD and Other Disorders Often Appear Together?
The reasons for the frequent overlap between BPD and other disorders are multifaceted. Shared genetic vulnerabilities can predispose an individual to emotional dysregulation, a core feature of BPD that also plays a role in anxiety and depression. Furthermore, the chronic emotional pain, unstable relationships, and identity disturbance common in BPD can naturally lead to feelings of hopelessness and despair, paving the way for a depressive episode. Similarly, the intense fear of abandonment in BPD can fuel the constant worry characteristic of anxiety disorders. Traumatic life experiences are another significant factor, often serving as a common root for both BPD and PTSD.
The Overlap: BPD with Depression & Anxiety
Distinguishing between the symptoms of BPD, depression, and anxiety can feel like trying to separate intertwined threads. The emotional turmoil of BPD often includes symptoms that look very similar to those of mood and anxiety disorders, which is why a careful understanding is essential.
When BPD Symptoms Mimic or Intensify Depression
The profound emptiness, mood swings, and suicidal ideation in BPD can be mistaken for major depressive disorder. A key difference often lies in the trigger and duration. While depression may involve a persistent low mood for weeks, the emotional shifts in BPD are typically more reactive and can change rapidly within hours, often in response to interpersonal events. When both are present, BPD's chronic emptiness can deepen depression's hopelessness, and its rejection sensitivity can trigger more severe depressive episodes. A free BPD test can help begin the process of identifying these specific patterns.
Recognizing Co-occurring BPD & Anxiety Disorders
Anxiety is a near-constant companion for many people with BPD. The intense fear of abandonment can manifest as generalized anxiety, while social anxiety can stem from an unstable sense of self and fear of judgment. Panic attacks are also common, often triggered by fears of being left alone. The impulsivity in BPD can sometimes be an attempt to escape this crushing anxiety. Recognizing that the anxiety is linked to core BPD fears is crucial for finding treatments that address the root cause. If you're questioning your symptoms, consider taking a BPD symptoms test.
The Impact of Dual Diagnosis on Treatment Pathways
A dual diagnosis of BPD with depression or anxiety significantly impacts treatment. An approach targeting only depression may fail if it doesn't also address BPD's underlying emotional dysregulation and interpersonal difficulties. The most effective treatment plans are integrated, often using therapies like Dialectical Behavior Therapy (DBT), which is designed to treat BPD but also includes skills for managing depression and anxiety. Acknowledging the full scope of your challenges allows for a more holistic and effective path to recovery.
BPD vs. Complex PTSD: Unpacking the Differences
The overlap between Borderline Personality Disorder and Complex Post-Traumatic Stress Disorder (C-PTSD) is one of the most confusing areas in mental health. Both conditions can arise from prolonged trauma and share many symptoms, making misdiagnosis common.
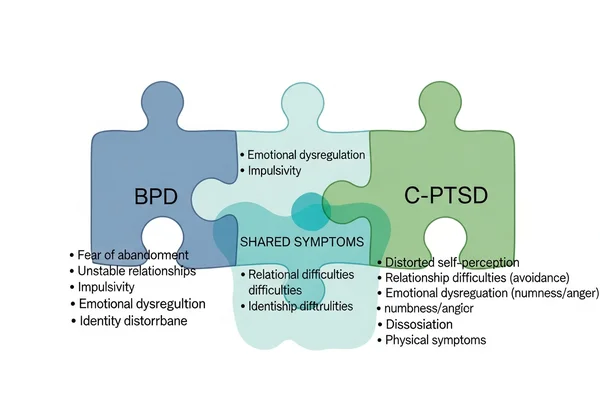
Shared Experiences: Trauma, Dysregulation, & Relationships
Both BPD and C-PTSD are rooted in trauma, especially prolonged developmental trauma like childhood abuse or neglect. As a result, individuals with either condition often struggle with emotional dysregulation, relationship difficulties, and a negative self-concept. They may experience emptiness, dissociation, and difficulty trusting others. These shared foundations explain why the symptoms appear so similar, validating the common confusion.
Key Distinctions in Diagnostic Criteria and Focus
Despite the overlap, there are key distinctions. The core of BPD, according to diagnostic criteria, is often centered on an unstable sense of self and an intense fear of abandonment. In C-PTSD, the core is more centered on the trauma itself; symptoms like flashbacks and avoidance are central, and the negative self-concept is directly tied to feelings of being damaged by the trauma. While someone with BPD may fear abandonment in any relationship, a person with C-PTSD might primarily struggle with trust due to past betrayals.
Effective Treatment Approaches for Both Conditions
Fortunately, many therapeutic approaches are effective for both conditions. Trauma-informed care is essential for anyone with a history of trauma. Modalities like DBT are highly effective for the emotional dysregulation in BPD, while therapies like Eye Movement Desensitization and Reprocessing (EMDR) are excellent for processing the traumatic memories central to C-PTSD. Often, an integrated approach provides the most comprehensive healing.
Navigating Diagnosis: Why a Comprehensive Approach is Key
Given the complexity of BPD comorbidity, self-diagnosis can be misleading. True clarity comes from a professional evaluation that considers all facets of your experience, which is the most effective step for your long-term well-being.

Seeking a Professional Evaluation for Complex Symptoms
If you suspect you have BPD with overlapping symptoms, seeking a formal evaluation from a qualified mental health professional, such as a psychiatrist or psychologist, is the most important step. They have the training to conduct a thorough diagnostic assessment, which may include clinical interviews and standardized questionnaires. This process will help untangle your symptoms, leading to an accurate diagnosis and a tailored treatment plan.
How Preliminary Assessments Help Uncover Hidden Overlaps
While not a substitute for a professional diagnosis, a preliminary screening tool can be a helpful first step. A scientifically-informed BPD test can help you organize your thoughts and identify patterns. It offers a structured way to reflect on your experiences with emotional intensity, relationships, and self-image. Bringing these results to a professional can foster a more productive conversation. You can start your test today as a confidential step toward self-understanding.
Finding Clarity and a Path Forward with Co-occurring Conditions
Understanding BPD comorbidity isn't about collecting labels; it's about gaining a complete, compassionate understanding of your emotional landscape. Recognizing that BPD often travels with anxiety, depression, or trauma validates your experience and shows you are not alone in your complex struggle. This knowledge is power—it is the first step toward seeking targeted, effective treatment that addresses you as a whole person.
Recovery is not just possible; it is expected with the right support. A comprehensive diagnosis leads to an integrated treatment plan that empowers you with skills to manage emotions, build stable relationships, and create a life worth living. If this article resonates with you, speak with a mental health professional for a formal diagnosis, and consider using the free BPD test online offered by BPD Test as a confidential, insightful tool to begin your journey toward clarity and hope.
Frequently Asked Questions About BPD Comorbidity
Can BPD symptoms be mistaken for depression or anxiety alone?
Yes. The intense mood shifts, feelings of emptiness, and chronic worry in BPD can mimic standalone depressive or anxiety disorders. A thorough assessment focusing on symptom patterns, especially concerning relationships and self-image, is critical for an accurate diagnosis.
How do doctors differentiate between BPD and Complex PTSD?
Clinicians look for subtle differences. They assess if the primary driver is fear of abandonment and an unstable self-image (BPD) or if it's more related to trauma memories, avoidance, and a shattered sense of safety (C-PTSD). A detailed personal history is essential.
If I suspect I have BPD and other disorders, where should I start with treatment?
The best starting point is a comprehensive diagnostic evaluation with a mental health professional. Once you have an accurate diagnosis, a therapist can help you find an integrated treatment plan. Often, therapies like DBT are recommended first because they build a strong foundation of emotional regulation skills beneficial for all co-occurring conditions.
How accurate are online tests for identifying BPD when other conditions are present?
Online screening tools are preliminary educational resources, not diagnostic instruments. They help identify potential BPD traits that other conditions might mask, providing a valuable starting point for a conversation with a professional, but they cannot replace a clinical diagnosis. You can take our quiz to explore your symptoms.
Is it possible to recover from BPD if I also have co-occurring disorders?
Yes, recovery is absolutely possible. Effective treatment for BPD, such as DBT, is designed to be holistic and provides skills that directly help manage symptoms of depression and anxiety. Treating co-occurring disorders simultaneously with a comprehensive plan often leads to the best long-term outcomes.